Tuesday, January 31, 2006
Treatment of Peripheral Lymphedema by Microsurgical Anastomoses of Lymphatics with ValvularVein
Lisheng Li Weigang Gao Shanliang Wang Tisheng Chang
Abstract Objective
Lymphatic microsurgery has been one of the top choices in the treatment of obstructive lymphedema of extremities that are not responsive to conservative method. The major drawback of this method is the possible blood reflux from vein to lymphatics after lymphatics-vein anastomoses. To keep the one way flow at the lymphatics-vein anastomoses site, We explored a new way to anastomose the lymphatics with the adjacent valvular veins with patent valve.
Methods
Fifty-six cases (16 postmastectomy arm lymphedema, and 40 leg lymphedema) with chronic limb lymphedema underwent lymphatics-vein shunts by microsurgical anastomoses of lymphatics with valvular vein either from adjacent veins at the obstructed area or autogenous vein grafts from the distal segment of the V. Saphena magna or/and its collateral branches in the medial surface of the leg. Results The patients were followed up for 12 to 56 months. A moderate elastic support was generally applied to the affected limb postoperatively. The study demonstrated very good results in 57% of the patients(32 patients), good in 30%(17 patients)and fairly good in 9%(5 patients),null in 4%(2 patients) in the follow-up period of 12 to 55 months after lymphatic microsurgery.
Conlusion
Anastomoses of lymphatics with valvular veins have been proved clinically to be very effective with very good and good results in 87% of the patients (49/56) in our series of cases with chronic lymphedema of extremities. It is supposed that the existed valves in the vein may play an essential role in maintaining one-way flow of lymph through the lymphatics-vein anastomoses site after operation and attaining the steady results of lymphedema regression.
Key Words:
Chronic lymphedema; lymphatics-Vein anastomoses; microsurgical treatment
Journal Article Page
----------------
There is evidently extensive research being done in China on lymphedema. As I can find information and status studies, I'll post them. Interesting cutting edge research.
Pat
Thursday, January 26, 2006
Surgical procedures and lymphedema of the upper and lower extremity
Feb 2006
Millard Fillmore Hospital, University at Buffalo, Buffalo, New York.
BACKGROUND:
Lymphedema occurs in the upper and lower extremity, in a minority of patients, following axillary and groin dissections, respectively. Several technical operative factors have been implicated through the years whose relative significance remains unknown.
METHODS:
Retrospective review of the author's personal experience with axillary and groin dissections and review of the articles and results written on the author's series of patients. The results, specifically lymphedema, are reported in relation to components of each surgical procedure and the presence or absence of additional surgical procedures, e.g., wide excision of the primary site when performed in the distal leg.
RESULTS:
In the axilla, skeletonization of the axillary vein, dissection up to and including Level III nodes, removal of the fat and nodes above the level of the axillary vein (exposing the brachial plexus), removal of pectoralis minor and all the axillary fat, exposing thus serratus anterior, latissimus dorsi and subscapularis are all technical components which do not cause lymphedema. It seems excessively thin flaps in axillary dissections may be the most likely cause for upper extremity lymphedema. The incidence of upper extremity lymphedema, in our experience, after axillary dissection is low (2%).For the lower extremity, skeletonization of the femoral and iliac vessels, in continuity dissection of the femoral and deep nodes (iliac and obturator), do not cause in themselves lymphedema (which occurs in 30% of the patients). The incidence of lymphedema increases with making thin flaps, with wide resection of a primary melanoma below the knee, postoperative incidence of cellulites, failure to follow a prophylactic regimen of leg elevation and compression stockings, and obesity.
CONCLUSIONS:
Lymphedema in the upper and lower extremity may be caused by making thin flaps during node dissection, the additional wide excision of primary sites in the distal half of the extremity, postoperative cellulitis, and failure to follow an antilymphedema regimen.
J. Surg. Oncol. 2006;93: 87-91.
(c) 2006 Wiley-Liss, Inc.
PMID: 16425311 [PubMed - in process]
Tuesday, January 24, 2006
Laughter really may be good medicine

Reuters HealthFriday, January 20, 2006
By Amy Norton
NEW YORK (Reuters Health) - Sitting through a funny movie seems to be as good for your heart as running through the park, a small study suggests.
In an experiment with 20 healthy young adults, researchers found that participants' blood flow improved when they watched a movie that made them laugh. In fact, the circulation boost was similar to what's been seen with aerobic exercise, according to findings published in the February issue of the medical journal Heart.
However, that doesn't mean laughing should take the place of running, Dr. Michael Miller, the study's lead author, told Reuters Health. Instead, an "optimal scenario" might be to watch a funny movie while jogging on a treadmill, said Miller, who is with the University of Maryland Medical Center in Baltimore.
Exactly why laughing might give a jolt to the circulation isn't clear. It's possible that it counters the effects that stress hormones can have on blood vessel function, Miller and his colleagues speculate. In addition, laughter may spur the body's production of nitric oxide, a chemical that helps dilate blood vessels.
The study involved healthy men and women who submitted to several non-invasive measurements of blood flow in the arm's brachial artery. Dilation in this artery is a good indicator of blood flow to and from the heart.
The measurements were taken before and after participants watched clips from a comedy film, such as "Something About Mary," and from a distressing film, like "Saving Private Ryan."
On average, the researchers found, participants' blood vessel dilation was more than 50 percent better after the comedy than after the depressing film.
A number of studies have linked negative emotions, such as major depression and chronic hostility, to poorer heart health. Researchers have speculated that persistent elevations in stress hormones may be involved. But far less is known about the cardiovascular effects of positive emotions, according to Miller.
He said he hopes these findings will spark more research into how positive feelings influence heart health.
SOURCE: Heart, February 2006.
Laugh Lots - Shake those Lymphedema Limbs
Sunday, January 22, 2006
Rotator Cuff Surgery and Arm Lymphedema
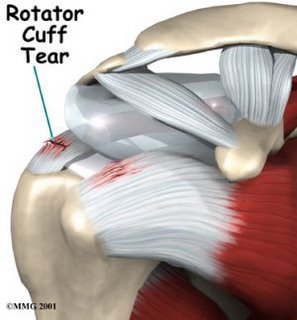 Sometimes surgery for rotator cuff problems are unavoidable, especially if you have an actual tear.
Sometimes surgery for rotator cuff problems are unavoidable, especially if you have an actual tear.What are the implications for those either at risk for or already have lymphedema?
Clinical studies indicate good sucess with this surgery. There appear to be the normal swelling post-op and even in lymphedema patients it usually subsides. See the initial article for a study done on this.
There are no studies on the at risk patient that I am aware of. From my own personal experience, an individual I know who is highly at risk for lymphedema (several family members have it) has experienced off and on swelling. It may be too early to accurately know what will happen.
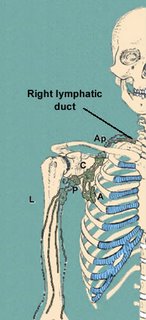
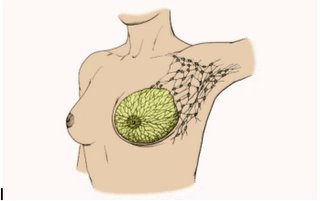
In either event, it is imperative that the surgeon understand the possibilities of lymphedema and understand the location of the lymph nodes in this area. Picture below give illustrations.
Lymphedema Preoperative Considerations:
1. For the prevention of infection and/or to lower the risk of infection it may be necessary for you to be on a preventative therapy of antibiotics BEFORE surgery.
2. For the prevention of blood clots (venous thrombosis) and based on any additional underlying medical conditions, you should also discuss the possibility of being on blood thinners before the surgery.
3. Make arrangements and plans for the scheduling and/or resumption of decongestive massage therapy for the lymphedema after the surgery.
4. Be sure to have your PCP, surgeon and lymphedema therapist working together to design a treatment/therapy modality that is best for you.
5. Familiarize yourself with the rotator cuff surgery so that you will know what to expect.
6. With consideration of surgical complications, it is important to try all methods of treatment before a surgery is planned.
7. What are the considerations of the need for a future second surgery affect your lymphedema.
8. If you are obese or morbidly obese discuss how the added strain of the surgery will affect your lymphedema.
9. Be sure to understand the specifics of what you can or can't do, how long you will be off work, financial arrangement and the need for personal assistance you may have.
Possible Complications
Complications include possible infections, especially around an the incision, damage to nerves or blood vessels and of special concern to those with lymphedema, the lymph nodes of the region.
General Patient Post-Operative Considerations Here are some do’s and don’ts for when you return home:
Do wear the sling every night for at least the first month.
Don’t use your arm to push yourself up in bed or from a chair because this requires forceful contraction of muscles.
Do follow the program of home exercises prescribed for you. You may need to do the exercises 4 to 5 times a day for a month or more.
Don’t overdo it! If your shoulder pain was severe before the surgery, the experience of pain-free motion may lull you into thinking that you can do more than is prescribed. Early overuse of the shoulder may result in severe limitations in motion.
Don’t lift anything heavier than a cup of coffee for the first 6 weeks after surgery. Do ask for assistance. Your physician may be able to recommend an agency or facility if you do not have home support.
Don’t participate in contact sports or do any heavy lifting for at least 6 months.
Contact your Physician if
Pain, swelling, soreness or redness in the arm Increase in shoulder pain Fever Discharge, pus or smelly drainage Sudden or unexplained re-swelling of joint (after initial post operative swelling has decreased) If the arm was not swollen before surgery, immediate report any post-operative edema.
These illustrations show which lymph nodes are in the general area and may be effected
The Surgery
Rotator cuff surgery is a highly technical procedure; each step plays a critical role in the outcome.
After the anesthetic has been administered and the shoulder has been prepared, a cosmetic incision is made over the top front corner of the shoulder.
This incision allows access to the seam between the front and middle parts of the deltoid muscle. Splitting this seam allows access to the rotator cuff without detaching or damaging the important deltoid muscle, which is responsible for a significant portion of the shoulder's power. All scar tissue is removed from the space beneath the deltoid and the acromion (part of the shoulder blade to which the deltoid attaches). Thickened bursa and the rough edges of the rotator cuff and humerus (upper arm bone) are also smoothed to make sure that they pass smoothly beneath the acromion and deltoid.
The edges of the cuff tendons are identified and the quality and quantity of the cuff tissue is determined.
The goal of the repair is to reattach good quality tendon to the location on the arm bone from which it was torn. If the tendon cannot reach this spot with the arm at the side of the body, the shoulder surgeon releases the tendon from the surrounding tissues. If good quality tendon will not reach its attachment site after these releases, the cuff tear is deemed to be irreparable. In this situation the useless tendon is cut out and the shoulder is again examined to assure smooth and full motion. Again, achieving this smooth movement may require trimming of the tendon edges or the bone of the upper humerus. Occasionally, it may be necessary to perform an acromioplasty, a procedure in which part of the bone overlying the rotator cuff is removed. Acromioplasty is avoided unless it is necessary because it increases the risk of weakening the deltoid and causing scar tissue.
If the rotator cuff is repairable, a groove or trough is fashioned in the normal attachment site for the cuff.
Sutures (lengths of surgical thread) draw the edge of the tendon securely into the groove to which it is to heal. This method of attachment leaves a smooth upper edge of the cuff repair to glide beneath the acromion and deltoid and avoids possible problems with suture anchors. After the cuff is repaired, the deltoid muscle and skin are closed.
Because the deltoid is not detached from the acromion in this surgical approach, it is called the "deltoid on" approach.
Anesthetic Rotator cuff surgery may be performed under a general anesthetic or a brachial plexus nerve block. A brachial plexus block can provide anesthesia for several hours after the surgery. The patient may wish to discuss their preferences with the anesthesiologist before surgery.
Length of rotator cuff surgeryRotator cuff surgery usually takes approximately one hour. However, the preoperative preparation and the postoperative recovery may add several hours to this time. Patients often spend two hours in the recovery room and about two days in the hospital after surgery.
Recovery of comfort and function after cuff surgery continues for a year after surgery.
Rotator cuff surgery is a major surgical procedure that involves cutting of skin, release of scar tissue, and suturing of tendons and bone. The pain from this surgery is managed by the anesthetic and by pain medications. Immediately after surgery, strong medications (such as morphine or Demerol) are often given by injection. Within a day or so, oral pain medications (such as hydrocodone or Tylenol with codeine) are usually sufficient.
Initially, pain medication is administered usually intravenously or intramuscularly. Sometimes patient controlled analgesia (PCA) is used to allow the patient to administer the medication as needed. Hydrocodone or Tylenol with codeine are taken by mouth. Intravenous pain medications are usually needed only for the first day or two after the procedure. Oral pain medications are usually needed only for the first two weeks after the procedure.
Pain medications can be very powerful and effective. Their proper use lies in the balancing of their pain relieving effect and their other, less desirable effects. Good pain control is an important part of the postoperative management.
Pain medications can cause drowsiness, slowness of breathing, difficulties in emptying the bladder and bowel, nausea, vomiting, and allergic reactions. Patients who have taken substantial narcotic medications in the recent past may find that usual doses of pain medication are less effective. For some patients, balancing the benefit and the side effects of pain medication is challenging. Patients should notify their surgeon if they have had previous difficulties with pain medication or pain control.
After surgery the patient spends an hour or so in the recovery room. A drainage tube is sometimes used to remove excess fluid from the surgical area. The drain is usually removed on the second day after surgery. Bandages cover the incision. They are usually changed the second day after surgery.
Recovery and rehabilitation in the hospital
Shoulder motion soon after rotator cuff surgery helps achieve best possible shoulder function. Shoulders with cuff disease may have substantial scarring and may be stiff. One of the major goals of rotator cuff surgery is to relieve any stiffness. However, after surgery scar tissue will tend to recur and limit movement unless motion is started immediately. This early motion is facilitated by the complete surgical removal of the scar tissues so that after surgery the patient needs only to maintain the range of motion achieved at the operation.
A continuous passive motion (CPM) machine is often used to gently move the shoulder in the recovery room immediately after surgery. The CPM, shown in figure 6 and movie 1, is continued for the first few days after surgery whenever the patient is in bed.
During the hospitalization, the patient learns a simple rehabilitation program that will be used to maintain the range of motion at home after discharge.
Figure 7 shows the exercises used to maintain elevation and rotation of the arm. On the day of surgery or on the day after, the physical therapist teaches the patient gentle range of motion exercises. Usually, the patient is shown how to stretch the shoulder forward and out to the side, preventing stiffness and adhesions.
QuickTime movie
Movie 1: Continuous passive motion machine (1.70 MB)
Patients are discharged as soon as:
the incision is dry,
the shoulder is comfortable with oral pain medications,
the patient feels comfortable with the plans for managing the shoulder,
the patient can perform the range of motion exercises, and
the home support systems for the patient are in place.
Discharge is usually on the second or third day after surgery.
Walking and use of the arm (with the elbow at the side) for gentle activities are encouraged soon after surgery.
If a cuff repair has been performed, the arm must be used only with the elbow at the side and only for very gentle activities so that the repair is protected. These precautions remain in place for three months until the initial healing of the cuff repair is complete.
The patient's specific limitations can be specified only by the surgeon who performed the procedure. It is important that the repaired tendons not be challenged until they have had a chance to heal. Usually the patient is asked to lift nothing heavier than a cup of coffee (with the elbow at the side) for the first three months after the surgery.
Management of these limitations requires advance planning to accomplish the activities of daily living during the period of recovery.
Patients usually require some assistance with self-care, activities of daily living, shopping, and driving for approximately three months after surgery. Patients usually go home after this surgery, especially if there are people at home who can provide the necessary assistance, or if such help can be arranged through an agency. In the absence of home support, a convalescent facility may provide a safe environment for recovery.
Recovery of comfort and function after rotator cuff surgery continues for many months after the surgery. Improvement in some activities may be evident as early as three months. With persistent effort, patients make progress for as long as a year after surgery.
Effects of general health on healing
The healing after rotator cuff surgery can be compromised by smoking, poor nutrition, and medications such as cortisone. Diabetes can cause additional scar tissue. Heart and lung disease, as long as they are well managed, do not seem to have an effect.
See entire excellent section on the surgery:
For additional Information:
Wednesday, January 11, 2006
Prevention and Treatment of Rotator Cuff Tendonitis with Arm Lymphedema
Rotator cuff tendonitis is an increasing problem in our Western societies. Having improperly treated or untreated arm lymphedema can put you at more of a risk for this condition.
The swelling may cause:
1.) Added strain to the shoulder muscles, ligaments and tendons due to the weight and volume of fluid.
2.) Cause nerve and vascular compression from not only the swelling, but from tissue changes that occur in fibrosis (hardening).
3.) Result in infections and added inflammation of the shoulder.
It is thus very important that we understand how to prevent rotator cuff tendonitis from happening and/or learn to recognize it early before an actual cuff tear occurs necessitating surgery.
The best preventative steps will be in preventing lymphedema from starting or in diligent management if you already have it.
For the arm at risk of lymphedema:
Become familiar with and practice the 18 steps of preventing arm lymphedema and also the early signs of arm lymphedema. If you experience any of the syptoms in that article, let your doctor know immediately and as for a referral to a certified lymphedema therapis. Do what you need to do to try and prevent lymphedema from starting.
If you already have lymphedema:
1.) It is imperative that you be compliant with your prescribed treatment program Work with and in cooperation with you therapist to get that swelling down and keep it down.
2.) Be diligent and consistent with your home care and daily management which will include correct exercise, skin care, bandaging, and self massage.
Both groups should read the below articles and learn to recognize the early warning symptoms of tendonitis.
------------------------
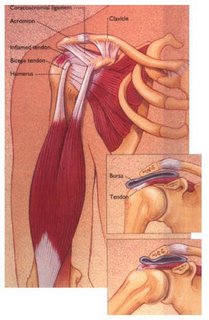
What is rotator cuff tendonitis?
Rotator cuff tendonitis, also knows as "bursitis" or "impingement syndrome" occurs when the rotator cuff gets irritated on the undersurface of the acromion. The reason this begins in the first place is a source of some debate: Some people are born with a "hooked" acromion that will predispose them to this problem. Others have rotator cuff weakness that causes the humerus to ride up and pinch the cuff. This means that the bursa - a water-balloon type structure that acts as a cushion between the rotator cuff and acromion/humerus - gets inflamed.
What are the symptoms of impingement syndrome?
Common symptoms of rotator cuff tendonitis include:
Pain - primarily on top and in the front of your shoulder.
Sometimes you can have pain at the side of your shoulder. Usually is worse with any overhead activity (reaching up above the level of your shoulder).
Weakness - mild to moderate weakness, especially worse with overhead activity.
Popping - sometimes bursitis that occurs with rotator cuff tendonitis can cause a mild popping or crackling sensation in the shoulder
Unable to sleep on shoulder - most patients complain of difficulty sleeping on the shoulder at night
How is impingement syndrome diagnosed?
Often, the diagnosis is suggested by your symptoms. Your orthopaedic surgeon or primary care physician can have you perform various maneuvers to detect this problem. This physical examination is designed to test your motion, strength, and certain positions of pain. In addition, plain x-rays can show a spur on the undersurface of the acromion. An MRI is occasionally ordered if a rotator cuff tear is suspected.
How do we treat rotator cuff tendonitis?
Just about all orthopedic surgeons agree that this problem should be treated initially "conservatively" - that means without surgery.
What are the steps to healing?
Stop any activities that can aggravate your symptoms. For example, if you're painting the ceiling in your garage and it's making your shoulder feel worse, stop doing it!
Do not ignore your body - it is telling you (with pain) that something is wrong.
Take medications, if necessary, to make you comfortable and decrease your pain.
Consider using cryotherapy (cold therapy) to get your pain under control.
STRENGTHEN your rotator cuff!
Why does strengthening the rotator cuff muscles work?
When you have this tendonitis you get into a "vicious cycle":
First your rotator cuff is irritated for various reasons (overuse, injury, etc).
Then it doesn't work as well - and that causes increased pressure under the acromion bone.
The only way the acromion can react to that is to make new bone (a bone spur!).
That bone spur then presses on the rotator cuff.
So the rotator cuff gets MORE irritated, and then more weak, and so on... (go back to step 1)
earlier in this article, many people have rotator cuff tears, but no symptoms of shoulder pain.
What is the initial treatment for a rotator cuff tear?
Because many rotator cuff tears do not need surgery, the initial treatment is usually with conservative measures. While the size of the tear may not change with conservative treatment, the symptoms often diminish. In some cases, usually a traumatic rotator cuff tear in a younger patient, early surgery will be recommended.
However, the standard treatment is to start with conservative measures.
The first steps of rotator cuff treatment include:
Physical Therapy
Physical therapy is the most important step in the treatment of a rotator cuff injury. Strengthening the rotator cuff muscles is important to maintain normal shoulder function. A few meetings with a physical therapist can help teach you exercises to help alleviate and prevent a recurrence of your shoulder pain.
Anti-Inflammatory Medications
Medications are most helpful at controlling the symptoms of a rotator cuff tear. Simple anti-inflammatory medications can be taken regularly for a short period, and then be used when symptoms of a rotator cuff tear flare up.
Cortisone Injections
Cortisone injections can be incredibly helpful at limiting the acute inflammatory process and allowing the patient to begin therapy. It is important to participate in the therapy and exercises even if the shoulder feels better after an injection. The therapy part of treatment will help prevent a recurrence of symptoms.
These steps may help to relieve pain and strengthen the muscles around the joint
What treatments are available if I still have symptoms?
These conservative measures may not be effective in all patients. In general, a good effort at conservative therapy is first attempted, especially in older patients or in patients who have chronic (long-standing) injuries. In younger patients who have an acute, traumatic injury, sometimes surgery is considered early as the likelihood that conservative treatment will help is low. Surgery is also considered in patients who have tried conservative treatment, and still have difficulty with their shoulder.
Rehab and Exercises
----------------
Information on the Shoulder:
Ortho Associates
Next - The Surgery
Wednesday, January 04, 2006
Rotator cuff tendonitis in arm lymphedema
Herrera JE, Stubblefield MD.
New York-Presbyterian Hospital and Hospitals of Columbia and Cornell, New York, USA.
OBJECTIVES:
To report rotator cuff tendonitis as a complication of lymphedema and to discuss the possible etiology and treatment options.
DESIGN:
Retrospective review of 8 cases.
SETTING:
University hospital outpatient clinic.
PARTICIPANTS:
A total of 8 breast cancer patients with a history of lymphedema and ipsilateral shoulder pain.
INTERVENTION:
Patients with lymphedema and ipsilateral shoulder pain were diagnosed with rotator cuff tendonitis if all of the following 3 tests were positive: supraspinatus test, Neers impingement test, and Hawkins impingement test. Patients diagnosed with rotator cuff tendonitis were prescribed a nonsteroidal anti-inflammatory drug (NSAID) and physical therapy (PT).
MAIN OUTCOME MEASURES:
Improvement in symptoms of shoulder pain at a 4- to 6-week follow-up, as measured by visual analog scale (VAS).
RESULTS:
Seven of 8 patients reported a subjective decrease in their symptoms of shoulder pain at a 4- to 6-week follow-up. The average improvement in shoulder pain as measured by VAS was a 4.5-point decrease from the original pain score given. One of 8 patients had a full-thickness supraspinatus tendon tear and required additional decongestive therapy and PT to obtain relief of symptoms.
CONCLUSIONS:
Rotator cuff tendonitis is a complication of lymphedema caused by internal derangement of tendon fibers, which may be subject to impingement, functional overload, and intrinsic tendinopathy. Conservative treatment with NSAIDs and PT is a safe and effective treatment.PMID: 15605330
[PubMed - indexed for MEDLINE]
.....................
Shoulder arthroplasty in patients with prior mastectomy for breast cancer.
Andrews LR, Cofield RH, O'Driscoll SW.
Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN 55905, USA.
Twenty women, all of whom had undergone mastectomy for breast cancer and 11 of whom had undergone radiation therapy, underwent shoulder arthroplasty. Two of these patients subsequently underwent resection arthroplasty for delayed infection and uncontrollable instability. Seventeen patients were available for follow-up, which averaged 4.6 years (range, 23 months to 13 years). There was significant improvement in pain (P < .0001), with no pain in 8, slight pain in 7, occasional moderate pain in 1, and moderate pain in 1 of the patients. A significant improvement in active motion occurred only in external rotation. Active elevation increased 7 degrees, from 92 degrees to 99 degrees; external rotation increased 17 degrees, from 25 degrees to 42 degrees; and internal rotation increased 1 level, to L3. All patients were pleased with their results. Complications were frequent. Apart from the 2 patients who underwent reoperation, 5 patients with preoperative lymphedema experienced exacerbation of their edema and 2 others developed new lymphedema. The edema returned to prearthroplasty levels or resolved in all patients by 5 months. In addition, antecubital vein thrombosis occurred in 1 patient, delayed long head of biceps rupture in 2 patients, and late rotator cuff tearing in 3 patients. In carefully selected patients, shoulder arthroplasty can be effective in pain reduction, but little increase in range of motion should be expected. Complications (often involving soft tissues) are frequent. New or increased arm edema can occur; however, edema resolved or returned to prearthroplasty levels in our patients.PMID: 11075321
[PubMed - indexed for MEDLINE]
Monday, January 02, 2006
The Seven Habits of Highly Effective People

Habit 2: Begin with the End in Mind
Beginning with the end in mind is the habit of keeping your day to day focus on your whole life instead of on day to day things. What do you want people to say about you after your life is over? What kind of person do you want to have been. What is the legacy you want to leave? Habit 2 is the process of developing a clear answer to this question. This is your purpose in life. When you have a clear vision of your overall purpose in life, it is easy to solidly say "no" to some things and "yes" to others. It becomes easier to plan your year or this month or week or day. You constantly ask yourself: Does this align with what I ultimately want to do?
This habit means not talking about yourself during a conversation. It means wanting to experience something new from the other person, wanting to discover a new way of seeing the world, wanting to truly stand in the other's shoes and feel their unique pain and their unique joy. ACTION ITEM: When you notice that someone is speaking with negative emotion, this means they need to be listened to and understood. It means that there is something under the surface that will poison relationships, projects and communication until it is identified and addressed. When someone says, "This is stupid" or "I hate school" they mean something else besides "this is stupid" and "I hate school". Use your listening skills (respond, rephrase, repeat) to find out what it is that they really mean.
Habit 7: Sharpen the Saw
Sharpening the Saw means continually keeping yourself physically, intellectually, emotionally and spiritually fit. It means regularly jogging, swimming, reading a wide spectrum of books, continually learning new things, relaxing, vacationing, praying, and meditating.
Sunday, January 01, 2006
Lymphedema 2006

The new year 2006 has dawned and the old year is gone forever, nothing now but a memory. I hope everyone can look back and feel they did their very best without regrets and "what if's."
I am excited about the possibilities that lay ahead for all those with lymphedema, lipedema, lymphangiectasia and other related lymphatic conditions.
It promises to be a busy and progressive year for research into the causes and hopefully the cures of our conditions.
Some of the cutting edge research involves:
1. Tissue engineering to construct functional lymphatic tissue
2. Adipogenisis (how fat cells form) in lymphedema
3. The genetics of hereditary lymphedema and related syndromes
4. Study of the physiology of the lymphatic system - flow, pressure, valves, contractibility
5. Study of lymphangiogensis (how the lymph system forms) and how to use that to treat and cure lymphatic conditions
6. Study of the embryonic origina and development of the lymphatic system
7. Study of angiogenisis (blood vessel formation)
8. Further understanding of the role played by lymphatics in cancer
And perhaps the most important is an increased awareness and interest in understanding just how important the lymphatic system is to all other body systems and the major role it plays in our over health and other serious medical conditions.
Other important milestones for the furtherment of lymphatic research includes:
1. The Lymphatic Research Foundation recently introduced a LE Research Fellowship Awards Program
2. A renewed and ever increasing support from the National Institutes of Health
So with all that is going on to research, treat and cure lymphatic conditions, where does all this leave us as patients in 2006 in terms of our own personal lives?
If I could only say one thing, it would be "Make 2006 Count!" I hope we can all come to the point where we say, "I have lymphedema" not "Lymphedema has me."
I want to share some tips that have helped me. But, before I do, I also don't want anyone sitting there thinking "this guy just doesn't understand what it is like to have lymphedema," because the reality is that I do understand. I have never had a day without this condition and have had to face almost an unbelievable array of complications, including lymphatic cancer, from it. I understand how painful lymphedema can be physically and understand completely how devestating it can be emotionally.
Make 2006 Count
Take charge of your life
Resolve that you will not be the person who just reacts to what lymphedema does to you. Become proactive in managing lymphedema and in creating a life that has quality and meaning.
Be diligent in selfcare
Follow to the letter the requirements of your treatment with the therapists. Work with them, not against them. Be meticulus in skin care, bandaging, diet and all the other aspects of managment that will help control your condition.
Get your eyes off yourself
Reach out and help others. Decide to be a positive and healing force with other people. This is not just a quaint cliche for me, but I do honestly believe that there are worse things you can have then lymphedema and there are so many desperately sick and hurting people all around me that I wouldn't trade places with for even a second.
Dump selfpity
Sure, having lymphedema is the pits, but selfpity is one of the most destructive mind frameworks we can ever get into. It has healed no one, cured nothing and accomplished zero. What it does do is destroys you inside, makes you miserable and eventually you wind up thinking crawling away into a lonely black hole. Hmmm....that sounds like an exciting way to life, doesn't it?
Discover new interests
If lymphedema prevents you from doing an activity that you love, learn a new hobby or discover a new interest. Don't just dwell on your loss of ability, be determined that lymphedema is not going to make you stop doings things and enjoying life.
Educate yourself about your condition
Care enough about your well being to take the time to study and learn credible information about lymphedema. Don't just wait for someone to tell you about it, take the initiative to learn.
Get Involved
There is a new and growing interest in advocacy for lymphatic conditons. I want to encourage you to suppport and be active in the efforts of groups like the Lymphedema Stakeholders.
Be involved in helping pass legislation right in the state you live in that will assure proper diagnosis and treatment.
Challenging the Myths
One other major change going on in the lymphatic world is a movement to question and debunk some of the myths that we have come to accept over the last couple decades.
Myth One - You can not be active with lymphedema.
I was so totally shocked when I came online to the cyber lymphedema world to see just how many of us were afraid to do any type of physical activity. "Oh, that's terrible or dangerous, it is going to make the lymphedema wors," we were told. I for one am glad to see this myth challenged and gotten rid off. It is a simple medical fact that exercise and activity are crucial to our our all mental and physical health. Not to mention that fact the exercise helps move fluids out of our bodies.
Myth Two - You really can not know what the true facts are about lymphedema.
Someone actually said that to me recently. That told me two things about this person.
First, they didn't care enough about themselves to try to learn.
Secondly, they have just surrendered to what they consider the proper "hopelessness" of lymphedema.
The problem isn't that there is a lack of credible information out there. The problem is that there is so much misinformation being presented. Everyone has their own clinically unproven concept of treatments, complications, diets, medicines etc...and even some lymphedema sites themselves are guilty of providing faulty information.
Go to websites that have proven their dependability. Some of these include The Lymphatic Research Foundation, Lymphovenous Canada, Lymphoedema Association of Australia, The Vodder School of Therapy, Pub Med and the National Lymphedema Network.
When you do research, visit the online libraries of medical schools, search out online medical journals. These all have solid information.
When someone says they know of a treatment, a herb, a technique...ask them for evidence, demand independent clinical studies that prove their claims.
Don't just believe what someone says or what you see written on a website.
Let's look forward to 2006 with expectations.....hopes for treatment and a cure.....hopes for a better life, right where we are.....
Remember
Life is meant to be a celebration of what we can do...not a requiem for what we can not.
